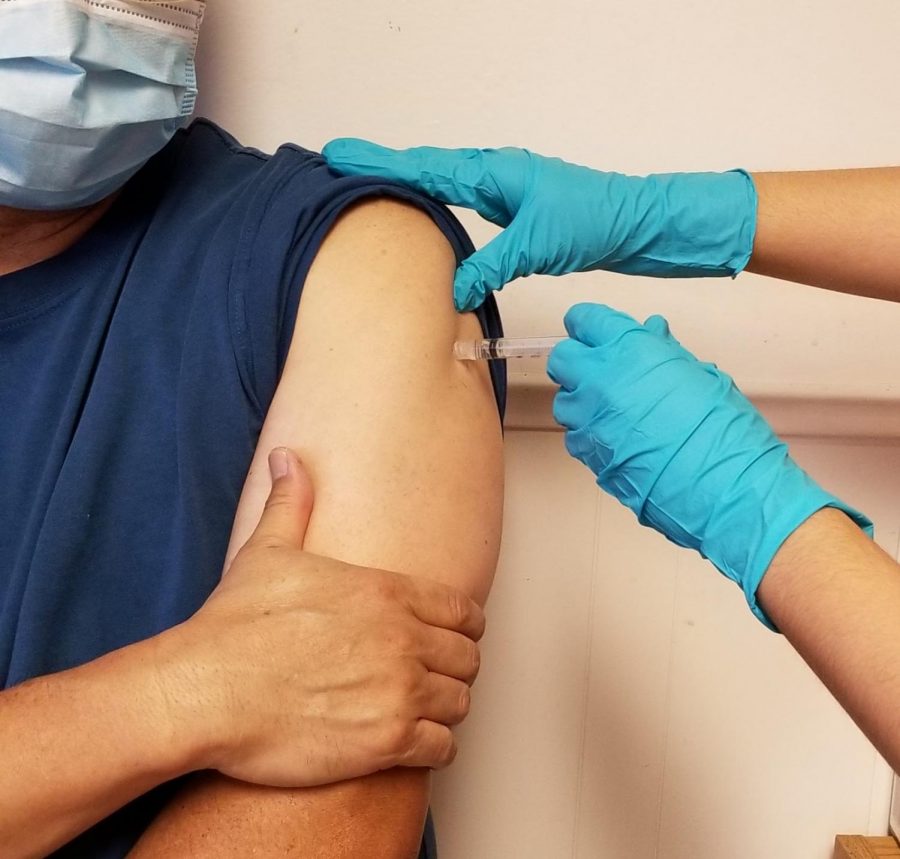
Pfizer Vaccine: Good News Amidst the Pandemic
Art/Photo by Alexssa Takeda
Despite all the negative events this year has brought, Pfizer and BioNTech offer a spark of hope with a vaccine that seems to be effective against COVID-19. “It was unexpected that the effectiveness would be that high,” Ms. Cortina commented. “If this assessment is accurate, the vaccine can go a long way towards ending the pandemic.”
November 20, 2020
The U.S. recently surpassed a record-breaking 11 million total COVID-19 cases at an unprecedented rate, with one million recorded in less than a week. But there seems to be a light at the end of the tunnel as Pfizer and BioNTech announced their vaccine seems to be 90 percent effective against the novel coronavirus.
Starting in July, Pfizer initiated Phase 3 clinical trials, which blindly tested over 43,538 healthy individuals, randomly assigning them either the vaccine or an inactive placebo. It is standard in clinical trials for only an independent board to know who received which treatment to ensure there is no bias. According to Pfizer and BioNTech, 94 out of 44,000 participants contracted the virus. Based on the early analysis, their mRNA-based vaccine candidate was 90 percent effective against COVID-19 in those who did not have prior evidence of the virus.
Compared to other vaccines, this is good news. For instance, influenza vaccines are 40 to 60 percent effective because of how often it evolves from year to year. Furthermore, the two companies have reported no serious safety concerns. In May, they ran tests on four versions of the vaccine to specifically detect any warning signs that might prevent them from continuing to test on a larger group. In the end, they chose vaccine version BNT162b2, which was reported to have fewer cases of side effects such as mild fatigue and headaches.
When this unexpected announcement was made, many individuals were thrilled, such as West High Biology teacher Mr. Patel. He expressed, “I was ecstatic about the announcement because I know that vaccines can take an extended period of time to develop. After hearing that the vaccine has been [90%] effective, it gave me an even better outlook on the future.” He further explained that this good news could give others hope and show that progress is being made. The vaccine’s success was especially surprising because of the approach Pfizer and BioNTech took to creating it.
The vaccine is mRNA-based, which means instead of using weakened strains of the virus, it uses small parts of the virus’ genetic information to trigger an immune response in the cell. This will tell the cell to create antibodies that will fight against the virus protein. This factor makes it easier and faster to produce the vaccine, allowing Pfizer to accelerate development. However, this technology comes with challenges. One of the most glaring is the way it must be stored. West High Biology teacher Ms. Cortina explained the issue: “This vaccine will need to be kept very cold, as in -70 degrees C cold. This will make the vaccine‘s distribution logistically difficult since very few facilities, outside of hospitals, research universities, and drug companies, have these freezers.” In addition, this type of vaccine is new, meaning no mRNA vaccine has ever been approved by the Food and Drug Administration.
Another obstacle is that only about half of Americans have indicated that they would take the vaccine once it becomes available, as shown in a CNN poll. Mr. Patel explained how this might cause complications for the general public: “If there are individuals who don’t get vaccinated, it’s possible that the virus could mutate. If it does mutate, the antibodies created from the original vaccine may not work.” In turn, this could leave many people vulnerable to new strains of COVID-19.
Some people don’t trust the vaccine due to the short period of time it was produced in. Many of them are concerned about adverse effects. A large amount of testing must be completed. As Ms. Cortina points out, “It is based on the result from only 90+ infections ― not a tremendously large sample size ― and the study hasn’t been going on long enough to know if there are any long term side effects.” She explained that Pfizer and BioNTech released a small amount of data to apply for Emergency Use Authorization, which would allow the vaccine to be distributed.
Still, the trial must continue until it reaches 164 cases of COVID-19 and an additional two months of observed safety data. Unanswered questions remain, such as how long immunity will last, or if the virus will stop infection. While the results offer evidence of an effective vaccine, success is still not certain.
If the vaccine were to be authorized, healthcare workers and high-risk patients are at the top of the priority list. The general population is predicted to get the vaccine closer to the middle or end of 2021. In a news briefing, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, emphasized that this news does not mean people should let their guard down: “Now we need to double down on the public health measures as we are waiting for the vaccine to come and help us out.” In other words, continuing mask-wearing, hand-washing, and social distancing is a must, especially as coronavirus cases continue to rise.